Is vision therapy covered by insurance? This question sparks curiosity as we delve into the intricacies of insurance coverage for vision therapy. From understanding what vision therapy entails to exploring insurance options, this topic offers valuable insights for those seeking vision care.
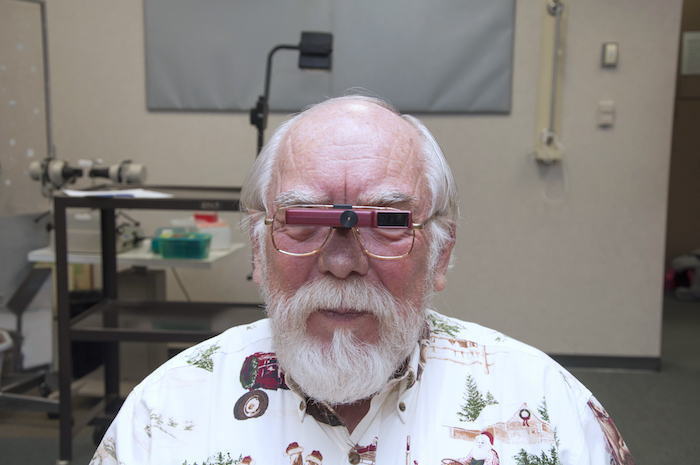
Vision therapy, a specialized treatment to improve vision, involves various techniques and exercises tailored to individual needs. It addresses conditions like lazy eye and crossed eyes, making it a vital aspect of eye care.
Understanding Vision Therapy

Vision therapy is a personalized program designed to improve visual skills and abilities. It involves a series of exercises and activities that aim to enhance eye coordination, focusing, and tracking. By addressing specific visual problems, vision therapy can help individuals improve their overall vision and quality of life.
Techniques and Exercises
- Eye tracking exercises: Activities that require the eyes to follow moving objects or patterns to improve tracking abilities.
- Eye teaming exercises: Tasks that help both eyes work together efficiently to improve depth perception and binocular vision.
- Focusing exercises: Techniques to strengthen the eye muscles responsible for focusing, aiding in near and distance vision clarity.
- Visual perceptual activities: Tasks that enhance visual processing skills, such as visual memory, visual discrimination, and visual closure.
Conditions Addressed by Vision Therapy
- Lazy eye (Amblyopia): Vision therapy can help strengthen the weaker eye and improve visual acuity.
- Strabismus (Crossed eyes): By improving eye coordination and alignment, vision therapy can correct strabismus.
- Tracking problems: Vision therapy can enhance eye tracking abilities, reducing issues with reading and other visual tasks.
- Convergence insufficiency: This condition, where the eyes have trouble working together at close distances, can be addressed through vision therapy.
Insurance Coverage for Vision Therapy
When it comes to vision therapy, many people wonder if their insurance will cover the costs associated with this type of treatment. Understanding the typical coverage provided by insurance companies for vision therapy, the factors that determine coverage, and the process of verifying insurance coverage can help individuals navigate this aspect of their healthcare.
Typical Coverage for Vision Therapy
- Insurance companies may cover vision therapy if it is deemed medically necessary.
- Coverage may vary depending on the type of insurance plan and provider.
- Some plans may cover a portion of the costs, while others may cover the full amount.
Factors Determining Coverage
- Medical necessity: Insurance companies typically require a diagnosis from a qualified healthcare professional to determine if vision therapy is medically necessary.
- Insurance plan: The type of insurance plan and provider can impact coverage for vision therapy.
- Policy details: Understanding the specifics of the insurance policy, such as coverage limits and requirements, is essential in determining coverage.
Verifying Insurance Coverage
- Contact your insurance provider: Reach out to your insurance company to inquire about coverage for vision therapy.
- Provide necessary information: Be prepared to provide information about the treatment, including diagnosis and recommended therapy plan.
- Check coverage details: Review your insurance policy to understand the extent of coverage for vision therapy.
Types of Insurance Plans
Insurance coverage for vision therapy can vary depending on the type of insurance plan you have. Here, we will detail the different types of insurance plans that may cover vision therapy and compare and contrast coverage between private insurance, Medicare, and Medicaid.
Private Insurance
Private insurance plans obtained through employers or purchased independently may offer coverage for vision therapy as part of their vision care benefits. Coverage can vary widely depending on the specific plan, so it is important to review your policy or contact your insurance provider to determine what is covered.
Medicare
Medicare is a federal health insurance program primarily for individuals aged 65 and older. While Medicare typically does not cover vision therapy for adults, it may provide coverage for certain eye care services related to medical conditions, such as cataract surgery or treatment for eye diseases. It is important to check with Medicare to understand what vision services are covered under your plan.
Medicaid
Medicaid is a state and federally funded program that provides health coverage to eligible low-income individuals and families. Coverage for vision therapy under Medicaid varies by state, with some states offering comprehensive vision care benefits that may include coverage for vision therapy services. It is recommended to contact your state’s Medicaid office to inquire about coverage for vision therapy.
Examples of Insurance Companies
Some insurance companies known to cover vision therapy include Blue Cross Blue Shield, UnitedHealthcare, Aetna, Cigna, and VSP Vision Care. However, coverage policies can differ between plans offered by these companies, so it is essential to verify coverage with your specific insurance plan.
Finding an In-Network Provider
Finding an in-network provider for vision therapy is crucial in maximizing your insurance benefits and minimizing out-of-pocket expenses. In-network providers have agreements with insurance companies to provide services at pre-negotiated rates, which can result in lower costs for patients.
Tips for Locating an In-Network Provider
- Check with your insurance company: Contact your insurance provider to obtain a list of optometrists or ophthalmologists that are in-network for vision therapy.
- Use online search tools: Many insurance companies offer online search tools on their websites to help you find in-network providers in your area.
- Ask for recommendations: Seek recommendations from friends, family, or your primary care physician for in-network providers that specialize in vision therapy.
Benefits of Selecting an In-Network Provider, Is vision therapy covered by insurance
- Cost savings: In-network providers typically charge lower rates for services covered by your insurance plan, reducing your out-of-pocket expenses.
- Insurance coverage: Services provided by in-network providers are more likely to be covered by your insurance plan, ensuring you receive the maximum benefit.
- Streamlined billing process: In-network providers are familiar with the billing procedures of your insurance company, making the claims process smoother and more efficient.
Last Point: Is Vision Therapy Covered By Insurance
In conclusion, the coverage of vision therapy by insurance is a crucial consideration for many individuals seeking vision improvement. By understanding the nuances of insurance plans and finding the right provider, one can access the benefits of vision therapy with ease.
Detailed FAQs
Is vision therapy covered by all insurance plans?
Insurance coverage for vision therapy varies among different plans. It is essential to check with your specific insurance provider to determine coverage.
What factors influence insurance coverage for vision therapy?
Factors such as the type of insurance plan, medical necessity, and individual policy details can affect coverage for vision therapy.
Can Medicare or Medicaid cover vision therapy?
Medicare and Medicaid may offer coverage for vision therapy in certain cases. It is advisable to check with your plan for more information.